Navigating Provider Data Challenges in Mental Health
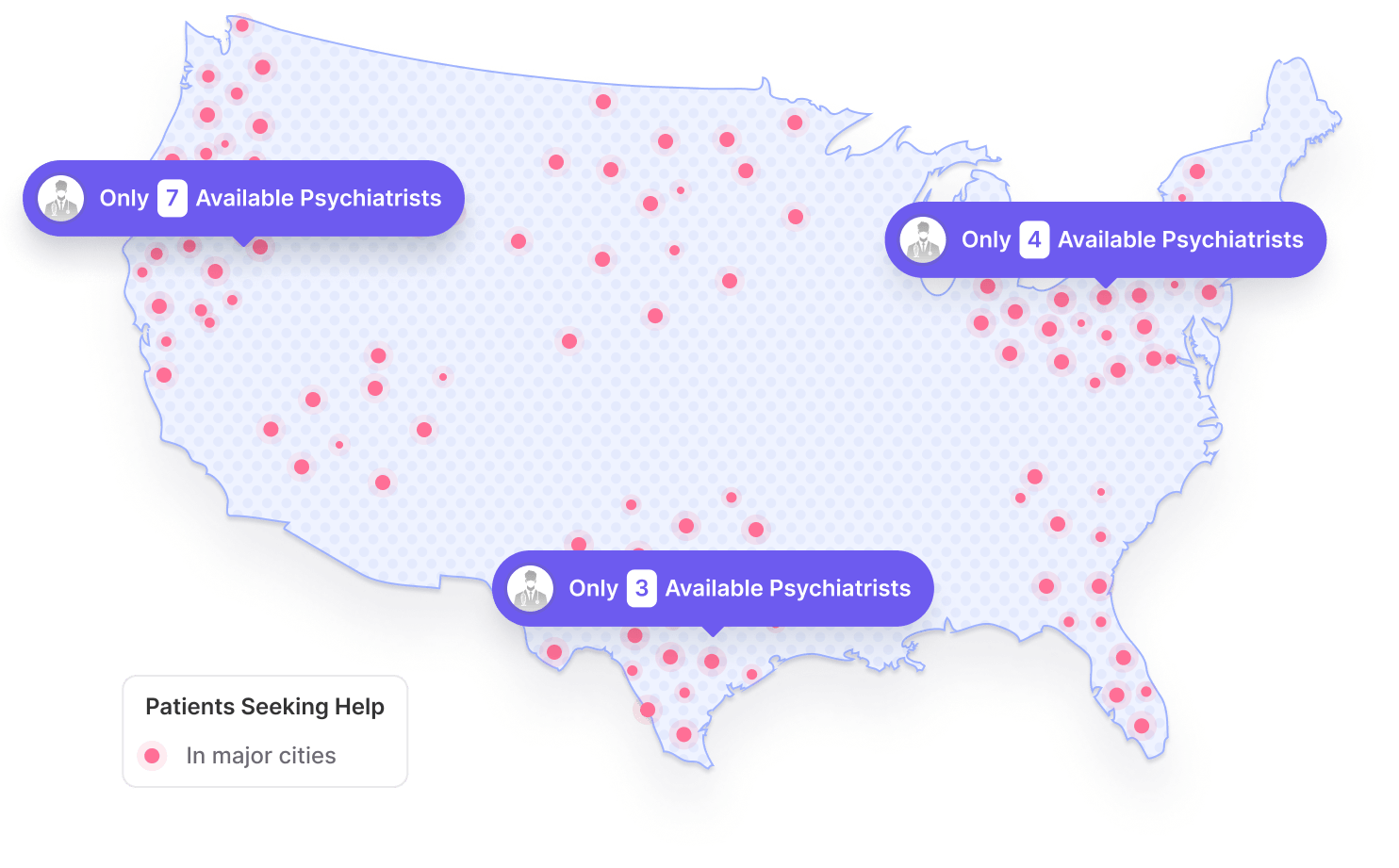
A New York State Attorney General report revealed that 86% of listed in-network mental health providers were not available or not in-network.

The "Ghost Network" Problem
“Ghost networks” — lists of providers who are marked as in-network but are actually unavailable, unable to accept patients, or do not take the advertised insurance — pose a significant barrier to mental health care access.
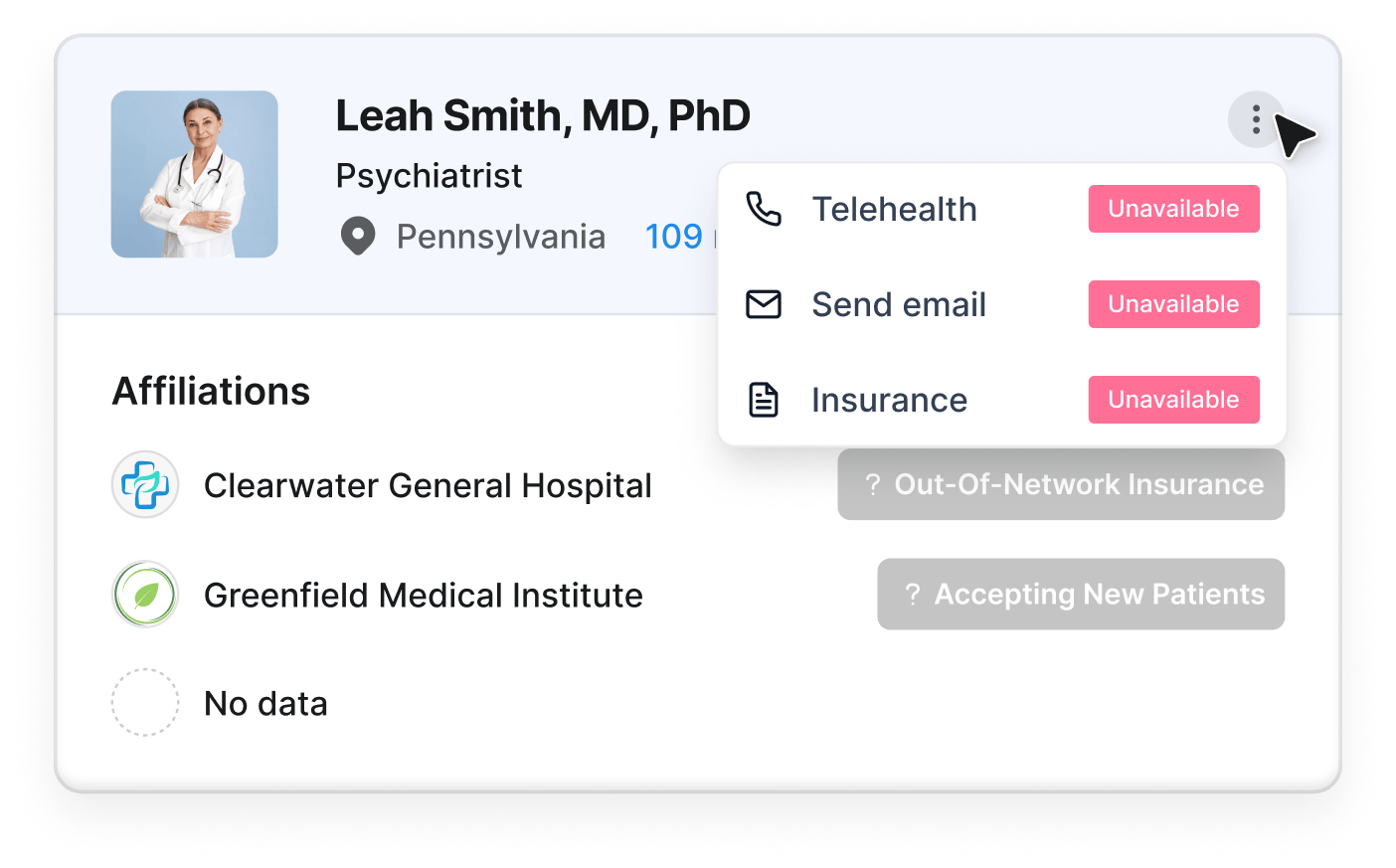
Inaccurate provider directories pose significant barriers to accessing mental health services. A study published by The American Journal of Managed Care found that 13.8% of psychiatrists and 9.1% of non-physician mental health professionals (NPMHPs) were listed outside their actual counties, while 8.6% and 7.2%, respectively, were listed as accepting new patients but were not. Incorrect contact details affected 6.6% of psychiatrists and 6.9% of NPMHPs, with inaccuracies in 33.4% of psychiatrists and 30.5% of NPMHP listings. These errors stem from frequent changes to provider details, inconsistent verification, complex insurance networks, and resource constraints in mental health services.
A New York State Attorney General report revealed that 86% of listed in-network mental health providers were either unreachable, not accepting new patients, or inaccurately listed as in-network. Out of 396 calls, only 56 appointments were successfully scheduled, highlighting the significant barriers created by these inaccuracies. A national survey similarly found that 53% of privately insured patients encountered directory errors, leading to out-of-network bills and delays in care.
This issue has drawn increased scrutiny, with a recent class-action lawsuit against Anthem Blue Cross Blue Shield of New York further spotlighting inaccessible in-network providers. A secret shopper survey revealed that only 7 out of 100 listed providers were accepting new patients with Anthem insurance, forcing many patients to pay out-of-network costs or face delays in receiving mental health services. Ghost networks force patients into costly out-of-network options, causing delays and financial burdens. The plaintiffs are asking Anthem to overhaul its provider directory in order to prevent further harm to subscribers, and if they prevail, the court might order Anthem to do so.

Factors Complicating Access to Care
A shortage of mental health professionals compounds the issue, with more than half of counties lacking a psychiatrist or addiction specialist. States like Wyoming and Utah have 96% and 83% of their populations, respectively, in provider shortage areas.
Misunderstanding among patients about the roles of different mental health providers adds to this challenge. For example, 22% of respondents in one survey could not access specialty mental health care, with 53% of these individuals instead relying on primary care providers for mental health needs due to confusion about specialty options. Additionally, many patients do not understand distinctions between mental health providers, often seeking psychotherapy from psychiatrists, who often primarily manage medications.
94.7% of behavioral health providers work in solo or small practices, with 84.1% of psychiatrists working independently. This reality makes it difficult to track their practice details. Many payer directories lack details on telehealth availability, leaving patients without clear guidance on remote access.
Patients experiencing acute mental health crises are particularly affected by provider directory inadequacies: many mental health providers aren’t trained on how to support patients considering suicide and many hospital emergency departments have a shortage of beds for patients in crisis.
For providers, directory inaccuracies also pose financial burdens. According to the Council for Affordable Quality Healthcare (CAQH), providers spend an estimated $2.76 billion annually on directory maintenance, a cost that diverts resources from patient care and new patient outreach.
How Mental Health Care Navigation Companies Can Help
To improve access to mental health care, payers and care navigation companies can tackle directory inaccuracies and scheduling delays in the following ways:
Frequent Directory Updates: Regularly updating provider availability, location, and contact information — using real-time tools and outreach — helps minimize inaccuracies and reduces patient obstacles.
Expanding Network Reach: Establishing partnerships with top mental health providers offering services like Intensive Outpatient Programs (IOP) and Partial Hospitalization Programs (PHP) expands referral networks and better matches patients with suitable providers.
Transparency in Provider Records: Clearly labeling in-network and out-of-network providers and indicating accepted insurance plans can reduce patient frustration and increase transparency.
Overcoming Licensing Barriers: Staying informed on state-specific telehealth licensing requirements, as highlighted by the Medical Insurance Exchange of California (MIEC), and collaborating with other providers to navigate these challenges can broaden service areas and improve patient access in underserved regions.
Candor Solution
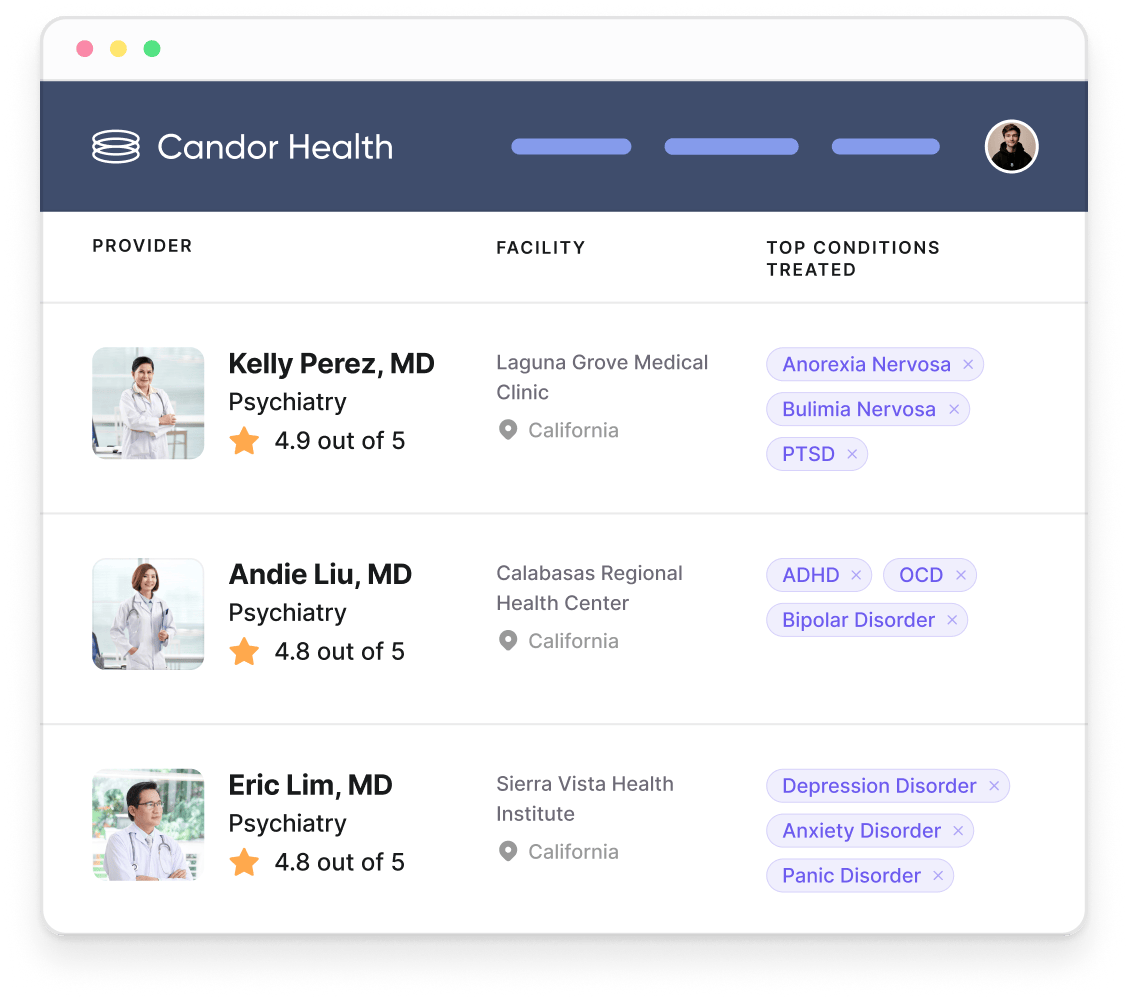
Candor Health’s platform contains details on locations, availability, and services for more than 1.5 million mental health providers, including psychologists, psychiatrists, therapists, counselors, mental health nurse practitioners, and social workers. By consistently updating provider information, removing inactive providers, and verifying insurance acceptance, Candor helps reduce the chances of patients encountering unreachable or unavailable providers.
With Candor Clinical Expertise, care teams can further refine searches for providers with experience in specific conditions like Obsessive-Compulsive Disorder or Bipolar Disorder, improving targeted access to care. Candor also has information on providers practicing in-person, only offering telehealth, or offering both care modalities.
For organizations expanding into new areas, Candor provides direct contact information to facilitate referral partnerships. Online booking links allow patients to schedule their own appointments, reducing administrative delays and supporting access to real-time availability.
More Posts

Case Study: How Sana Benefits Scaled Care Navigation

The Overlooked Bottleneck of Provider Data Accuracy

Provider Data Accuracy Without Compromising Network Adequacy
